Overview
As an employer, it’s your responsibility under the Occupational Health and Safety Act to take every precaution reasonable in the circumstances to protect a worker. This guide will help you use current public health and workplace health and safety information to develop a plan and put controls into place to help make the workplace safer for everyone.
All employers are encouraged to develop a COVID-19 workplace safety plan and to review and update it regularly. You can use the COVID-19 workplace safety plan template to help create your plan.
Some businesses, including all those operating during a lockdown or shutdown, must have a written safety plan by law. Check Ontario.ca/COVID-19 regularly for updates. If you are required to have a safety plan you must make it available to anyone who asks to see it, and post it in a place where it will be seen easily.
Employers are not required to send their plan to the Ministry of Labour, Training and Skills Development and the ministry will not provide comments on safety plans sent in. During an inspection of your workplace, an inspector or compliance officer could ask whether you have developed a safety plan and may ask to see it.
Discuss and share your safety plan with everyone at work, including:
- workers
- unions
- supervisors
- health and safety representatives or members of joint health and safety committees (JHSCs)
- contractors
- suppliers
This guide does not replace the Occupational Health and Safety Act or the Employment Standards Act and their regulations and should not be used as or considered legal advice. Health and safety inspectors and employment standards officers apply the law based on the facts in the workplace.
Develop your COVID-19 safety plan
Key sources of information
It’s important that you talk to workers and your JHSC members or health and safety representatives, if any, for their input on the plan. Share the plan with all workplace parties when it is done. This will help ensure your workers and others understand how you plan to manage the risks of COVID-19.
Check the resources to prevent COVID-19 in the workplace for sector-specific information and examples of controls that apply to your type of workplace. These documents may be helpful as you develop your plan. Visit the webpage regularly to check for the latest information.
Make sure you continue to follow any provincial requirements under the Reopening Ontario (A Flexible Response to COVID-19) Act and any local public health orders.
Understand COVID-19 risks
The first step to control risks in a workplace is to identify them. For COVID-19, the risks are related to how the virus spreads.
COVID-19 can be spread at the workplace in two main ways:
- person to person, by people who are in close contact
- by surfaces or objects, when people touch their face with contaminated hands
The key risk factors for COVID-19 transmission include:
- prolonged exposure – spending more time with potentially infected people
- close proximity – working close to others
- crowded places – having more people in a space
- closed spaces – indoor spaces less fresh air (working indoors is riskier than working outdoors)
- forceful exhalation – activities that cause people to breath more deeply, such as exercise, speaking loudly and singing
The risk of severe health outcomes is not the same for all workers. The risk increases with age and is higher for people with certain medical conditions.
It is possible for COVID-19 to be spread by people who do not have any symptoms. Act as if everyone is infected when setting up controls.
Control COVID-19 risks in the workplace
Control measures are the steps you take to reduce the risks to your workers. With an infectious disease like COVID-19 your controls can help to break the chain of transmission of the virus and reduce the risk of a workplace outbreak.
Employers should implement a variety of measures to control potential exposure to COVID-19. Examples include:
- screening
- physical distancing and barriers
- good ventilation
- frequent cleaning and disinfection of surfaces
- source control masking
- personal protective equipment
In situations where one or more controls cannot be consistently maintained it is especially important that other controls are in place.
Use the hierarchy of controls
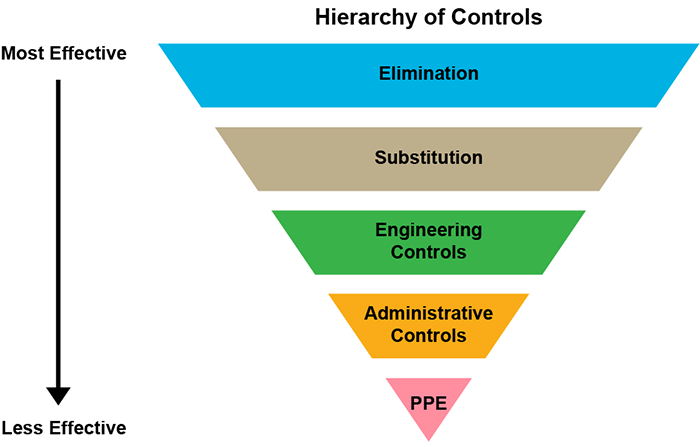
The hierarchy of controls (image and description below) can help you choose the right controls for your workplace. This applies to all workplace hazards, not just COVID-19.
The levels in the hierarchy of controls, in order from most effective to least effective, are:
- elimination
- substitution
- engineering controls
- administrative controls
- personal protective equipment (PPE)
When making your plan, always start by considering the most effective controls first. First, try to eliminate the hazard altogether. Where eliminating the hazard is not possible, use multiple engineering and administrative controls.
The higher the control appears in the diagram and the earlier it is in the list, the more effective it is. The first three types of controls are more effective because once in place they do not usually require additional action by a worker. The effective use of administrative controls and PPE requires workers and other people to implement them properly and consistently every time.
Even with the rapid and collaborative response to COVID-19, there are still many uncertainties about the disease. As new findings emerge, what we know about the risks and best practices for controls may change, so it is important to stay current. The safety plan approach allows you to incorporate new information as it becomes available.
Elimination
Remove the risk of exposure entirely from the workplace. For example, having everyone work from home all the time would eliminate COVID-19 risk from a workplace.
Substitution
Replace a hazardous substance with something less hazardous (for example, replace one chemical with another). For an infectious disease such as COVID-19, substitution is not an option.
Engineering controls
Make physical changes to remove the hazard through ventilation or separate workers from the hazard, including changes that support physical distancing and hygiene. For example, you could:
- install plexiglass barriers to separate workers from customers
- remove unnecessary doors that many people would have to touch
Administrative controls
Make changes to the ways people work and interact, using policies, procedures, training and signage. For example, you could:
- establish contactless curbside pickup
- create policies to limit the number of people in a space at one time
- schedule to stagger work shifts and breaks
- establish new cleaning and disinfection protocols
- provide education and training on proper hand washing technique
- set up a screening process
Personal protective equipment (PPE)
This is equipment and clothing worn by a worker to minimize exposure to hazards and prevent illnesses and infection. PPE is used to protect the wearer and can include such things as surgical/procedure masks and eye protection.
Correct use of PPE can help prevent some exposures, but it should not take the place of other control measures, for example, screening, hand hygiene, use of barriers and physical distancing where possible. PPE must be used alongside other control measures already in place.
Using masks as a control measure
A mask is a piece of equipment that covers the wearer’s nose, mouth and chin. It is fixed to the face with straps, ties or elastic, either behind the head or with ear loops.
For COVID-19 protection, masks can be used as workplace control measures in two ways:
- as source control: workers and visitors wear the mask to protect those around them
- as personal protective equipment (PPE): workers wear the mask (along with eye protection) to protect themselves
Not all masks are suitable for both purposes. You need to consider how you will use the mask in your workplace and make sure to select a suitable type of mask. Cloth masks are not PPE.
How effective masks are as a control measure depends on:
- the type of mask(s) used
- masks being worn properly and consistently
To help you decide what is right for your workplace, see using masks in the workplace for more information.
Safety plan questions
There are six questions you should think through as you develop your COVID-19 workplace safety plan, as found in the COVID-19 safety plan template. The information in this document will help you to think through the issues as you develop a plan for the unique situation in your workplace.
Question 1: How will you ensure all workers know how to keep themselves safe from exposure to COVID-19?
Provide clear information and instruction to your workers. Make sure they know what they need to do to protect themselves and others. Ensure they know how to follow the work and hygiene practices in your plan, including all new safety measures.
Set up or use your current internal communication systems to provide frequent reminders and updates. Use a variety of ways to reach your workers, such as:
- posting notices in common areas
- emails
- virtual team meetings
- intercom announcements
Keep up with public health and workplace safety guidance for COVID-19. Share new information as soon as possible.
Some things to consider:
- post information for workers and other people entering the workplace
- share information in all languages spoken by your workers, if possible
- provide information in ways that are easy to understand, like graphics, and use resources from the Ontario government
- remind workers about available social and mental health supports, and encourage them to use these resources
- share information to help your workers stay healthy while commuting and travelling as part of their work
- train and re-train on procedures
Question 2: How will you screen for COVID-19?
By keeping symptomatic workers and other people from entering, you can help to reduce possible transmission in your workplace. Know the symptoms to look for and plan for how you will screen workers and others who enter your workplace.
Make sure all workers know to stay home if they have symptoms that are new, getting worse or unexplained (for example, not caused by an existing condition).
Screen all workers for COVID-19 symptoms and other risk factors (for example, close contact to known cases, recent international travel).
Types of screening
Screening involves an assessment of information about symptoms and interactions that may result in higher risks of transmitting COVID-19.
Based on the result of the assessment, a decision is made about whether a person should be excluded from the workplace until they are further assessed and/or symptoms resolve.
There are two different types of screening:
- passive screening: people assess their own risk factors and make the decision themselves
- active screening: the results of the screening assessment are reviewed to determine whether a person may enter the workplace
Screen actively
Employers must actively screen every worker before they enter the workplace at the start of their shift as described in the instructions issued by the Office of the Chief Medical Officer of Health.
- Active screening may be done in person at the workplace or remotely using telephone, internet (online), email submission or an app prior to entry.
- Actively screen each person entering the workplace for work purposes, including workers, volunteers, suppliers and contractors.
- Screening should occur before or when the person arrives at the workplace at the beginning of their shift or visit.
- Use the COVID-19 screening tool for workplaces or ensure that your screening process includes all the questions from the screening tool.
- A screener (or automated system) should advise anyone who does not pass the screening:
- that they may not enter the workplace, including any outdoor, or partially outdoor, workplaces
- to go home to self-isolate immediately
- to contact their health care provider or Telehealth Ontario (1-866-797-0000) to find out if they need a COVID-19 test and for further instructions
Make sure any screeners receive information and instruction on how to perform this work safely and what to do if a person must be excluded from the workplace.
You can also:
- screen visitors and clients by phone or through an app before they arrive for their appointment
- consider actively monitoring workers for symptoms more than once during their shift
Use signage
- Post clear signage at all entrances with the screening questions and instructions.
- If active screening of non-workers entering the workplace is not possible (for example, public transit, grocery stores), post signage instructing people with symptoms not to enter.
Encourage workers to self-monitor
- Encourage workers to monitor their own symptoms at all times.
- Ensure workers know where to find the online COVID-19 self-assessment tool.
- Ask workers to use the tool at home if they have any symptoms and to follow the instructions.
- Ensure workers know who their workplace contact is and how to get in touch with them in case the self-assessment, public health or their health care provider suggests they self-isolate, or if they start to experience symptoms at work.
Question 3: How will you control the risk of transmission in your workplace?
COVID-19 can be spread by people who do not have symptoms. This is why it is very important to have effective control measures in the workplace.
Examples of controls to consider are provided below. You can find many other ideas in the sector-specific resources to prevent COVID-19 in the workplace.
To operate your business more safely and to keep it operating, you may need to make changes to the workspace and to the ways your work is done.
Maximize physical distancing and separation
The most effective way to reduce the risk of COVID-19 transmission is to maintain physical distancing. Where possible, workers should continue to work from home and meet virtually until public health authorities advise otherwise.
To enable workers to maintain a physical distance of at least 2 metres from other people in the workplace, use a variety of engineering and administrative controls such as:
- barriers, such as plexiglass, to maintain separation as a primary means of control
- scheduling and other administrative changes to reduce the number of people who must share the same space including during shifts, lunch and other breaks providing adequate space by using and repurposing all available areas inside your facility and in the surrounding outdoor space
Source control masking
Using masks as source control involves having workers, visitors and clients in the workplace wear a mask to help protect those around them. All employers should consider using source control masking combined with other control measures.
Masks are especially important indoors and help to reduce the risk in situations where physical distancing cannot be consistently maintained.
Source control masks should not be used as a substitute for physical distancing – both control measures lower risk and should be used together. Consider:
- How effective using masks as source control may be in your workplace. This will depend on the type of mask(s) used and whether they are worn properly and consistently.
- Encouraging clients, customers and visitors to your workplace to wear face coverings (for example, non-medical mask, cloth mask) to help protect your workers and to reduce the risk of transmission of COVID-19 in your community.
In some workplaces in Ontario, wearing a mask or face covering may be required by public health or other authorities. You should be aware of the most current:
- requirements of the local public health unit
- relevant bylaws in the municipality in which you do business
- requirements under the Reopening Ontario (A Flexible Response to COVID-19) Act that are applicable to your business
- directives issued by the Chief Medical Officer of Health that are applicable to your industry or business
Even with other controls in place including physical distancing and source control masking, there may be situations where PPE will be required. A surgical or procedure mask worn as part of required PPE also works as source control and would normally meet any requirements for face coverings.
Ventilation and air flow
The risk of COVID-19 transmission is higher in more enclosed and crowded spaces. You should ensure that air-handling (HVAC) systems are maintained according to the manufacturer’s instructions and consider standards, such as those from the CSA and American Society of Heating, Refrigerating and Air-Conditioning Engineers (ASHRAE).
Additional steps you can take:
- use portable air cleaners
- keep windows and doors open as much as possible, including in colder weather
- adjust HVAC systems to increase the amount of fresh air and reduce recirculation
- continue ventilation and air exchange after regular business hours
- use available outdoor space whenever possible (for example, for meetings, breaks, client interactions such as curbside pick-up)
- consider going beyond minimum standards if possible
If fans are needed for temperature control make sure you are using them as safely as possible.
Reduce transmission from surfaces and objects
The virus that causes COVID-19 may be transferred to surfaces or objects. Workers can be infected if they touch their face with contaminated hands.
Consider the policies and procedures you can put in place to make sure you are cleaning and disinfecting and keeping the workplace as free of the virus as possible. The public health recommendation is to clean and disinfect high-touch surfaces at least twice a day.
To reduce transmission:
- identify commonly touched surfaces and commonly used areas in your workplace and put into place a schedule to clean and disinfect them
- consider whether there are high-touch surfaces that may need to be cleaned and disinfected more often
- assign tools, equipment and workstations to a single user if possible, or limit the number of users
- regularly clean and disinfect any shared equipment and tools, including between users
Support good hand and respiratory hygiene
The same everyday steps recommended by public health officials to stop the spread of COVID-19 are important in the workplace too. One of the most important things we can all do is to wash our hands often with soap and water.
Think about what you can do to make it easier for your workers to take these steps regularly at work. You can:
- post reminders to wash hands, use proper cough and sneeze etiquette and avoid touching eyes, nose or mouth
- provide ways to properly clean hands by providing access to soap and water and, if that is not possible, alcohol-based hand sanitizer
- ensure that workers can clean their hands frequently and whenever needed
- have all workers and visitors properly clean their hands before entering the workplace and after contact with objects and surfaces others may have touched
Personal protective equipment
To determine when personal protective equipment (PPE) is needed in your workplace, you will need to assess all the relevant factors in the workplace. This includes how effective the other control measures you have in place are. Even with other controls in place, including physical distancing and source control masking, there may be situations where PPE will be needed.
Correct use of PPE can help prevent some exposures, but it should not take the place of other control measures – PPE must be used alongside other control measures already in place.
It’s important that any PPE workers use is appropriate for the purpose. The effectiveness of PPE depends on every person wearing it correctly and consistently. Make sure your workers are trained on the care, use and limitations of any PPE that they use.
The Chief Medical Officer of Health has provided direction to health care organizations about the minimum requirements for COVID-19 PPE.
Where PPE for COVID-19 is needed in non-health care settings:
- it will likely consist of a surgical or procedure mask in addition to eye protection (such as face shield or goggles)
- gloves will not usually be needed as they do not provide any more protection than hand washing or using hand sanitizer
- it will not likely include a respirator (N95s and equivalent alternatives). These are only required in specific circumstances, for example where aerosol generating medical procedures are performed.
Workers that wear PPE for protection against workplace hazards besides COVID-19 must continue to use that PPE as required. This includes gloves for new cleaning and disinfecting products that workers use because of COVID-19.
Supplies of some types of PPE are limited. Make sure you are using the right controls to protect your workers and only using appropriate PPE so there is enough available for other workers who need it.
Question 4: What will you do if there is a potential case of, or suspected exposure to, COVID-19 at your workplace?
There are steps that you will need to take if one of your workers, visitors or clients has symptoms that may be related to COVID-19 or is diagnosed with COVID-19:
Step 1: Exclude the symptomatic person from the workplace
If a worker calls in sick, informs you of symptoms or informs you they had close contact with someone with symptoms, have them take the self-assessment. Ask the worker to follow any recommendations given by the tool, including being tested and self-isolating.
If anyone shows symptoms in the workplace, they should return home and self-isolate immediately. If they cannot leave immediately, they should be isolated until they are able to leave. Have a plan in place to deal with this and train supervisors on how to handle the situation.
If the person is very ill, call 911 and let the operator know that they may have COVID-19.
Ask the person to contact their doctor or Telehealth Ontario at
Step 2: Contact public health
Contact your local public health unit for guidance on what to do if someone develops symptoms at your workplace or you are told one of your workers has COVID-19. Public health will provide instructions and do contact tracing if needed.
To support contact tracing, have a system in place so you can provide information about which people had close interactions with an affected worker. This could include information such as:
- dates and times of interactions
- approximate length and frequency of interactions
- full names
- contact telephone numbers
- addresses (for workers) or the name of the visitor’s business
Step 3: Follow public health direction
Your local public health unit may require that:
- other workers who were exposed are notified and sent home to self-isolate, self-monitor and report any possible COVID-19 symptoms
- the workplace be shut down while the affected workplace or area and equipment are disinfected
- other public health measures are implemented
Disinfect surfaces that may have been touched by the ill person as soon as possible. Read Public Health Ontario’s COVID-19 fact sheet about cleaning and disinfection for public settings.
Self-isolation and return-to-work
Specific direction for each situation is provided by your local public health unit based on provincial guidance on the management of cases and contacts of COVID-19. Follow any and all public health direction.
Workers should self-isolate if they either:
- have symptoms
- had close contact with an individual with symptoms or a confirmed diagnosis
- have travelled outside of Canada
Close contacts may include people who have spent time less than two metres away from the infected person in the same room, workspace, or area without barriers or protective equipment and people living in the same home.
As an employer, it is important for you to understand the guidelines for COVID-19 self-isolation and return to work for your workplace. In general:
- A worker who had close contact with someone known to have COVID-19 should self-isolate for 14 days. If they do not develop symptoms, they may usually return to work and other activities 14 days after their last contact with the case.
- A worker with COVID-19 symptoms should self-isolate for at least 10 days from when the symptoms started.
- If a worker who has symptoms receives a negative COVID-19 test result, they may usually return to work before 10 days if they do not have a fever and their symptoms are getting better.
Some symptomatic workers may need to self-isolate for longer based on the advice of public health or their health care provider.
These timelines for self-isolation include time spent waiting for COVID-19 test results.
Consider how you can support workers so they are able to self-isolate and how you will manage if workers are unavailable. You could:
- assign work-at-home tasks to workers who must self-isolate
- use flexible schedules that allow self-isolating workers to work additional hours when they return to the workplace
- identify workers within your organization who can work additional hours or shifts as needed and make sure they are trained to do the work they might be asked to do
- develop back-up schedules that can be quickly implemented if needed
Workers who are considered employees under the Employment Standards Act have the right to take unpaid, job-protected infectious disease emergency leave if they must self-isolate because of COVID-19.
You cannot penalize an employee in any way for taking or planning on taking an infectious disease emergency leave.
Workers who must take time off from work because of COVID-19 may be entitled to employment insurance benefits or to other federal government financial supports. For information, visit the federal government’s website or contact Service Canada’s Employment Insurance Automated Telephone Information Service at
Step 4: Inform any workers who may have been exposed
You must let workers know if they may have been exposed in the workplace.
You should give all workers information about the date and time of the potential exposure and where it took place. Don’t give out any information that might identify the infectious person.
You do not need to undertake contact tracing activities unless asked to do so by your local public health unit.
This duty to inform your workers is independent of any public health direction, although it may be fulfilled by steps taken under public health direction as part of contact tracing.
Step 5: Report to Ministry of Labour, Training and Skills Development and the WSIB
If you are advised that one of your workers has tested positive for COVID-19 due to exposure at the workplace, or that a claim has been filed with the Workplace Safety and Insurance Board (WSIB), you must give notice in writing within four days to:
- the Ministry of Labour, Training and Skills Development
- the workplace’s joint health and safety committee or health and safety representative
- the worker’s trade union (if applicable)
Additionally, you must report any occupationally acquired illnesses to the WSIB within three days of receiving notification of the illness.
You do not need to determine where a case was acquired. If it’s reported to you as an occupational illness, you must report the case.
Question 5: How will you manage any new risks caused by changes to the way you operate your business?
Changes to work practices to prevent COVID-19 may affect the way you manage other risks in the workplace. For example, you may have controlled the risk of injury from lifting heavy items by having two people involved. This may not be possible while workers maintain physical distance.
It’s also possible that new procedures will bring new risks or challenges. For example, if you start using a new product for disinfection, you need to know what chemicals are in the product and how to use it safely. Workers may need new training.
Other plans and protocols you have in place may also need to be adapted for COVID-19. For example, how you will maintain physical distance during an emergency evacuation? What you will do if workers are told to self-isolate because of exposure to COVID-19?
Remote work may pose its own risks. This may include technological barriers, mental health concerns and ergonomic challenges.
New risks may be introduced by:
- workers having been away from their work
- changes to processes and procedures
- use of temporary labour and inexperienced staff
- restarting activities and machinery that have been shut down
- stress and change – consider how this affects your workers’ mental health
If your plan introduces shift work or splits teams that would normally work together, describe what steps you’ll take to:
- manage the impacts of shift work, including fatigue, transport, childcare and the potential dilution of skills available within a split team or rostered workgroup
- ensure each team has access to the right skills and support to be able to work safely
Question 6: How will you make sure your plan is working?
Operating a business during the pandemic and recovery stages will involve different ways of working. Checking to see how your plan is working will help you find the best solutions for your unique situation and adapt to any changes.
You may want to assign a manager or management team to take charge of COVID-related issues, including training for supervisors and regular dialogue with supervisors, to make sure there is compliance with all protocols. Use existing incident reporting systems. Schedule regular times to review your plan and its effectiveness.
Consider:
- How will your health and safety representatives or JHSC be involved in evaluating how well the plan is working?
- Add your COVID-19 measures and procedures to the JHSC checklist for required monthly inspections.
- In health care workplaces the joint health and safety committee or health and safety representatives must be consulted.
- What is the best way to engage your workers and workplace parties? Ask them how they would like to participate in decision making and provide feedback. Remember it may not be possible for them to complete forms or attend meetings outside of work time.
- What can you measure and monitor so that you can evaluate how well the new protocols are being followed?
- How will you communicate changes to processes, ensure all workers know about the changes and are trained to implement them?
- How often will you update and share new versions of your plan?
As the COVID-19 situation evolves what is right for your situation may change. Make sure to review and update your plan regularly.
